To provide a greater understanding of the Medicare-Medicaid enrollee or “dual eligible” population, CMS developed profiles that examine this population’s demographic characteristics, utilization, and spending patterns on a state-by-state basis. All 50 state profiles can be found here.
You can download California’s profile, but here is a closer look at the data compiled about the state’s dual eligible beneficiaries. The primary data source for the tables below is linked Medicare and Medicaid administrative and claims data for persons age 18 and older from calendar year 2007.
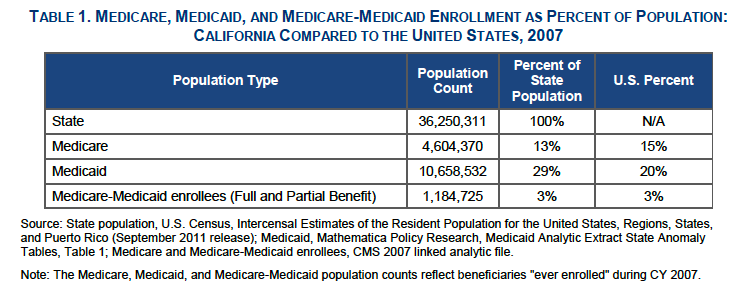
Total Population
Eligibility
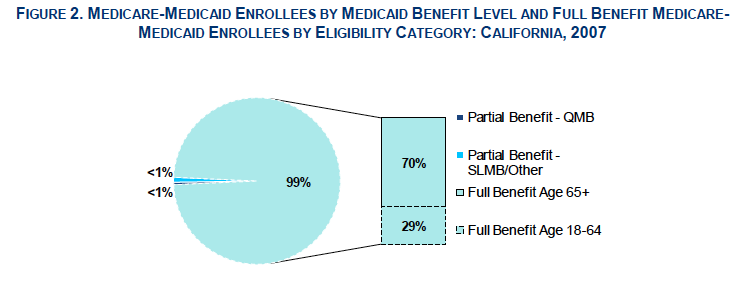
In California, 99% of dual eligible beneficiaries had full Medi-Cal benefits: 70% were ages 65 and older and 29% were ages 18 to 64. The remaining “partial benefit” enrollees received Medi-Cal help with Medicare premium payments and/or Medicare cost-sharing.
Demographics
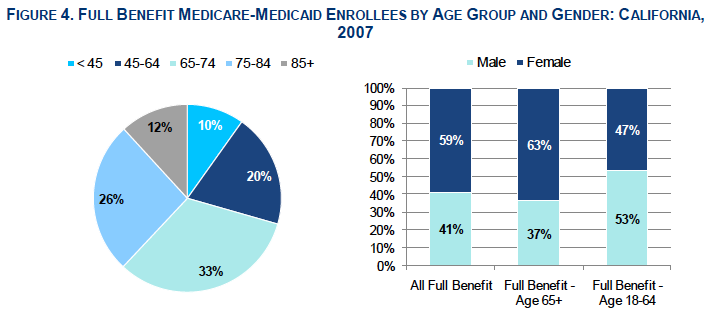
A total of 71% of full benefit enrollees in California were age 65 and older; people age 85 and older comprised 17% of this group. The majority of full benefit enrollees in California were women, particularly among the 65 and older group.
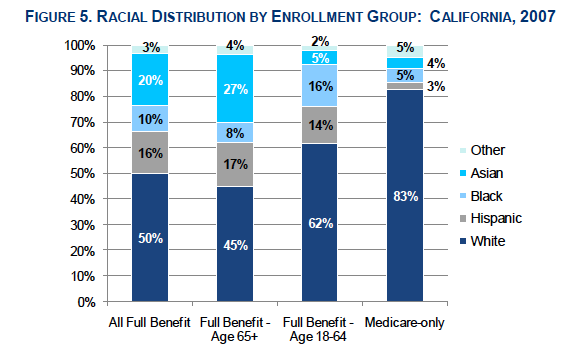
The dual eligible population is racially diverse. More full benefit dual eligible enrollees were non-white compared to the Medicare-only population.
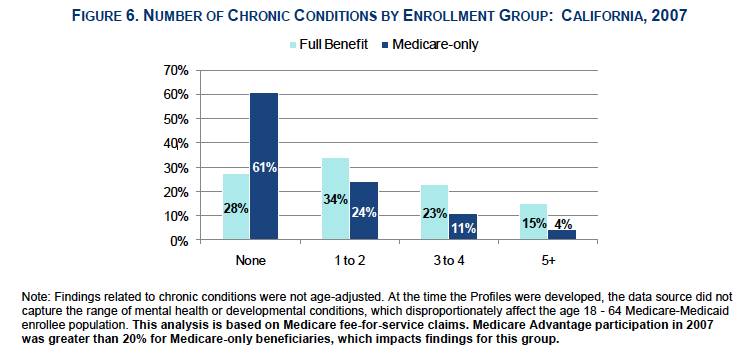
Chronic Conditions
Dual eligible beneficiaries have numerous chronic health conditions and tend to be sicker than the the Medicare-only population. Dual eligible enrolless were 3.5 times more likely than Medicare-only beneficiaries to have had 5 or more chronic conditions.
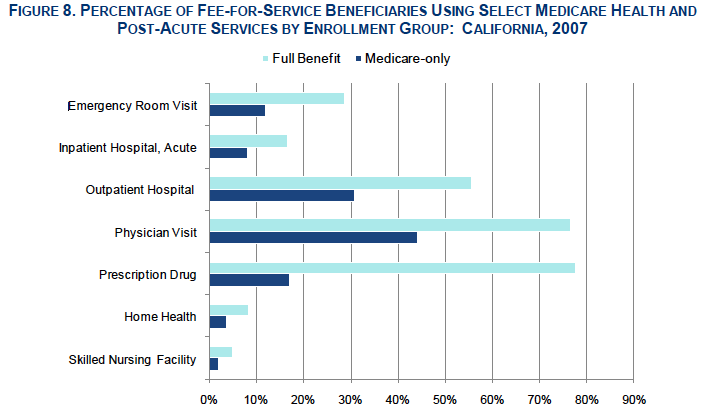
Utilization
Dual eligible beneficiaries have, on average, greater health and long-term services and supports (LTSS) needs than beneficiaries who have only Medicare or only Medicaid coverage. Dual eligible beneficiaries accounted for a disproportionate share of total utilization and spending in both programs.
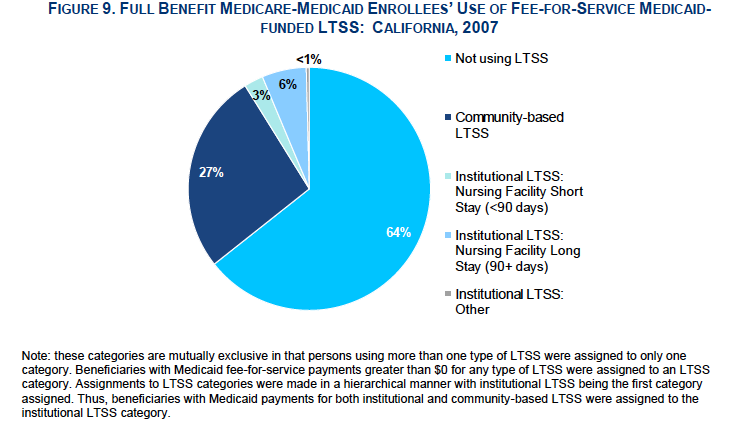
The majority of dual eligible in California did not use Medi-Cal-funded long-term services and supports. Of those who did, 75 percent used community-based LTSS and the remainder used institutional long-term care.
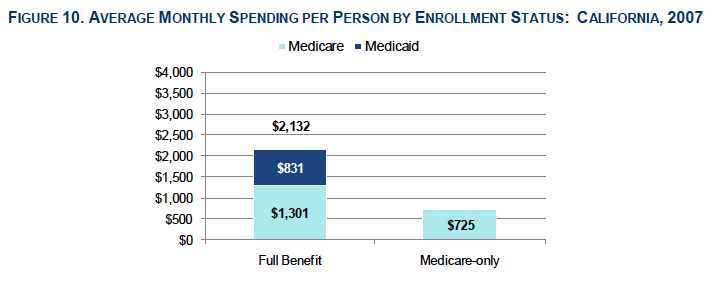
Spending
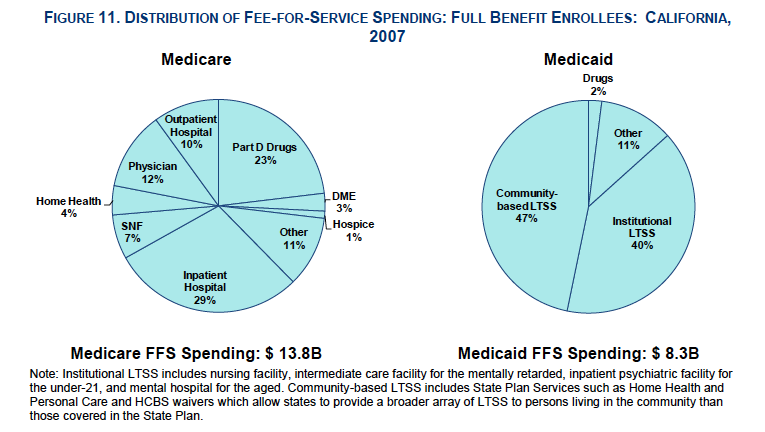
Dual eligible beneficiaries had significantly higher average monthly spending per person compared to Medicare-only beneficiaries, including higher average Medicare costs. Total costs included managed care and fee-for-service payments. The largest share of dual eligible beneficiaries fee-for-service Medicare spending went toward inpatient hospital care, whereas the largest share of fee-for-service Medi-Cal spending went toward long-term care services.

As an independent agent who specializes in low income seniors, it is very frustrating to find a way to reach Spanish speaking seniors. Today all low income Seniors (Dual) in Los Angeles should be receiving the best medical care available at no cost or very low cost. Knowing that I can provide this service for them only makes this job more frustrating.
I have been in the skilled nursing industry since 1977. With all the changes we have been through-nothing scares me more than this. I understand the need to take more cost effective measures-but to go live in 8 counties (including LA???) all at one time with so many mostly elderly medi-cal recipients is way too big a jump at once. I have seen in the last couple of years-the confusion and fright and misunderstandings caused by the Ventura County Gold Coast program(most recent MediCal managed care transition) and LA Care and other MediCal Managed Care plans. We had one very scary incident where a pt that had been in our SNF for over a year, got enrolled with LA Care in error-while she was out at a Dialysis Clinic awaiting her turn. They verified benefits-found the issue-were refusing to do the dialysis because they were not contracted, the transportation company was refusing to bring her back for the same reason and the doctor was refusing to get involved as the information was showing a new Primary MD who of course had never seen her-so he would not help.
Sending paperwork to these elderly folks explaining that they need to choose a plan or they will be auto enrolled is a waste of paperwork. They mostly will not read or understand any of this and many will go through what happened above.
There will also no doubt be serious interruptions to providers cash flow in an industry where we have been hit with cut after cut after cut and are still expected to provide quality care. There will be so much uncertainty, so much training to be done within the plans and among providers-once the rules are even known.
Way too much too fast-I am frightened to see the outcome.
Thank you for voicing the concern that many of us feel. I am horrified to think of what will happen when this plan becomes effective. Something needs to be done to stop this. I just wish I knew what that could be.
Ilook at the counties that have been choses to parcipate and understand why, (high population of seniors and disabled) but what about rule counties we face a whole different set of conditions. We do not have specialist, have to leave the county for disalysis, transporation to doctors is some times a whole days travel just to see the nearest doctor.Rule counties will not be in the systen until maybe 2016.By then the standards for CCI will already have been determined.
I wish someone could point me to a real live person who enrolls providers so that we can start helping these people. My frustration lies in the fact that I have submitted inquiries and W9s to several of the health plans 4-5 times with no follow-up from them. We want to be a provider but it seems impossible to connect with someone who can help us. Got any ideas?
I am 61 and have severe obstructive sleep apnea that wasn’t diagnosed by my health clinic for over a decade. I had the classic symptoms and all the primary care givers I had could not even write in my medical chart why I was seeking medical care because I could not sleep longer than 90-120 minutes before waking and woke in the morning with headaches. This went on for years and in 2005 again returned trying to find the cause of why I was so extremely sleepy during the day. Then when my body was completely collapsing from years of not sleeping with no problems falling asleep just kept on waking they still could not write my symptoms in my medical records. None of my primary care doctor looked at my past medical records they had in 2010 when I returned because I kept on falling asleep in just a couple of minutes the doctor mentioned a sleep test that she was going to order but again none of the doctors follow thru with doing the paperwork and nothing happened. 9 months later I had to ask an assistant “what happened to my sleep test?” and she ordered the test from an outside sleep center. This was when I learned the horrible truth about my illness that should have been diagnosed for 9 years and wasn’t. The doctor did not order the follow-up CPAP titration and the only way anything got done was by sending in writing a complaint about where and when and the medical center could not even keep and get a copy of the test that I finally had to give them. The doctor could not even put my test into my file and did not explain anything about the test. I had to be my own doctor and THANK GOD FOR THE INTERNET SO YOU CAN RESEARCH YOUR OWN ILLNESS BECAUSE TODAYS DOCTORS DO NOT KNOW ANYTHING AND DO NOT EXPLAIN ANYTHING. They do not even know Medicare rules. If I had listened to what the doctor told me I still would not have received my equipment for my illness. Then the doctor could not write and read the report and she wrote the wrong Rx and could not justify why the specialist who read my report ordered a Bi-pap which requires more detailed documentation because my doctor knew nothing and refused to refer me to a specialist for treatment. I finally became so frustrated by the extreme lack of any concern by this new young doctor I left and used my Medicare benefits and located a specialist on my own and absolutely NEVER TELL A DOCTOR YOU HAVE MEDICAID BECAUSE THEY WILL NEVER TAKE YOU AS A PATIENT. I just tell them I have Medicare. My specialist could not write correct medical information and the errors in my file and she did not listen when I informed her that there had been absolutely NO IMPROVEMENT AND I WAS GETTING WORSE. I left her for a second opinion.This specialist told me immediately on looking at my sleep test results that NO CPAP PRESURE HAD BEEN FOUND THAT WOULD DO ANY GOOD AND CPAP WAS NOT GOING TO HELP. My first specialist failed to follow Medicare rules that state “only rental of three months is permitted if NO IMPROVEMENT TO JUSTIFY BI-PAP” and the rental is to stop so that the machine is never purchased by Medicare and another medical solution needs to be found. Doctors do not listen to a thing you say and I now inform doctors I am voice recording and confirming everything in writing and reported this doctor to Medicare as Fraud for spending $10,000 from Medicare for a machine that does not help. This is why Medicare is costing the government Billions of dollars for treatments that doctors do not care if they make you better. When I got my medical file copy the errors she put in my file were unbelievable and totally false and I have filed a bad doctor claim to California Medical Board who doesn’t give a damn because doctors are never punished for bad medical care. It is a total MYTH that conservatives say they need TORT REFORM FOR FRIVOLOUS LAWSUITS AGAINST DOCTORS. You cannot get any attorney to take your case because people do not have the money to take a bad doctor to court and it has to be on contingency and unless it is iron clad it doesn’t get filed. Doctors should have to pay back the government if they give you treatments that do not work. Our whole system is messed up the way it pays. If they think they are going to coordinate care my California Medicare/Medical Managed health plan from Contra Costa cannot even answer my complaints I have written about and cannot even follow simple instructions I have repeatedly told them because of the severity of my illness because I have not received any specialist from them yet they cannot remember to call me after 2:30 p.m. because I am too ill and am not awake before that time to talk to them. This is why no person can call when I tell them and when you have a doctor that says you need a tracheostomy surgery because this is the only way I will get well and the health plan doesn’t answer your letter requesting this surgery. I am totally home bound because I fall asleep and should not drive because I do not get more than 90 minutes of sleep and I have filed and sent the paperwork in for IHSS and wrote on all my letters to them when to call and if they come to the house no one will answer the door so they have to just come in and go upstairs and wake me up because I fall asleep. No one did any of what I told them and they just “closed the file” because they cannot follow instructions and just let the disabled person get sicker and sicker and then they go to the hospital. This whole thing is going to come crashing down on them and God Help everyone. Kerry Pay kerrypaymann@gmail.com
I have been practicing for 7 years and I have 5 employees that rely on me. I read all of the comments above and I agree with all. Kerry so sorry about your situation, but there are good doctors out there who listen. I often limit the number of patients I have during the day, to make sure every pt has relieved quality care. However, this change will make everything more difficult and will lead to thousands of people having the same situation as Kerry. I currently deal with a handful of HMO and IPAs and getting authorization is an adventure. I often tell my patients that they have to wait. You know how horrible it is to tell someone in pain who is seeking your help to wait until their insurance allows me to do x-rays??? I often do them for free, but will not be able to sustain this. If the HMOs take over, nothing will be authorized. SCAN pays $45 for everything. If the doctor needs to do something beyond an office visit, they have to be fine with the $45 they will get paid for. I turn my scan patients away and they go to the hospital for their treatments. Unfortunately if this change happens I will be shifting gears, close my private practice and move to another state. It is sad because i really contribute to this economy. I have 6 employees, a medical biller, two rentals, and not to mention a line of retailers who rely on my to use their products (guaze, medicine…) in my office. Pharmacies need me to prescribe so that they can survive. Who ever thought about his program is not a doctor and has no idea how this will effect everyone.
What is worse is that really sick people will lose out more than anyone else. So sorry for everyone involve. I hate loosing my patients, as they have been part of my life for 7 years. I have seen their grand kids and kids, get married, graduate and have kids. That bond will be lost, and another doctor will take over. California is going to lose a ton of good doctors with this program. Good luck everyone.
One of the opportunities with a forum where commentators can post their issues, ideas or concerns yet distort the facts or misinforms the community is to have others like me respond to their veracity or motives in a respectful yet more complete and factual challenge.
Your posts begins with 7 years of practice, you’ve read and agreed to all the previous posts about the CA Dual Eligible Program, you limit your appointment patient load to a minimum so your patients receive excellent quality of your service and work with HMO’s and IPA’s and bemoan the $45 Office visit you get from SCAN and allege that getting authorizations is an adventure.
However, you failed to inform the community about your capitation and apparently you don’t understand how Medicare really works or you’re simply distorting the facts about how insurers like SCAN works in conjunction with your IPA’s.
So, if you had 500 Medicare patients with various Medicare insurers like SCAN and they all paid $45 for an office visit, your annual income would be about $270k, wouldn’t it? You’re paid every month regardless of seeing the patient. So, you’re thinking about moving to another state to sustain your practice because of this particular segment of your practice, really?
Almost all referrals are scheduled from the providers office and usually completed in a few minutes, so even if it’s an adventure it isn’t very long and I’ve never seen a provider personally schedule a referral, it’s always done by a staff member.
You also stated that you have seen generations of families in your practice, although you’ve been practicing for just 7 years. Respectfully, could you explain that assertion?
My point is your credibility and veracity is questionable based solely upon your posted comments and that is why I’m replying to your post.
You’re probably a great provider and God Bless you for your compassion and service, however, if you’re uninformed about how Medicare or MediCal really works, consult with a professional insurance agent who specializes in both areas (over 19 years experience for me) or another provider who has extensive experience and get the facts. I know you’ll be pleasantly surprised if you truly aren’t aware of how the system works.
Hi Harvey,
what specialty? My suggestion is to contract with the IPA/Medical groups. They are the link to participating health plans.
Question..Im 65..In 2014 will my non taxable social security be
counted against my eligibility for medicaid?? Im on medicare,but
could use help in paying my part b premium with Kaiser. i receive 1521.00 and 105.00 is then deducted for part ‘B”
Am i eligible for medicaid??..thank you, Tim
You will need to speak with your local county social services to discuss your Medi-Cal eligibility. You can find that information here.
call http://www.sscincorporated.com/ they might already be partnered with your health plan to help you enroll in a dual eligible program that can help subsidize your premiums and open the door to a number of free state/fed programs.
I am a dual eligible who is having a hard time wrapping my head around the fact that I am going to be herded into a program of which I want no part. I have been lucky enough to have enjoyed excellent health care all of my life____always fee-for-service. Perhaps that’s one of the reasons that I am extremely healthy today.I have seen people in HMOs getting short shrift, receiving second and third rate, substandard care and I’ve known of people who died unnecessarily. I’ve always known what HMOs are and how they work and I’ve always thought it was a disgraceful way to operate a health care delivery system.
Since my freedom of choice is being snatched from me, I can’t help but wonder if this is my punishment for the crime of being poor. Lumping everyone into one category is tantamount to one size fits all medicine, a practice I abhor because it doesn’t allow for individual differences and it doesn’t make good medical sense.
I will be going into this with a very negative attitude and a very large chip on my shoulder because I’m quite certain it will be deleterious to my health.
You should not worry and no one can force you…, you have a choice to opt-out from the program right away.
You can notify CMS right away and get your fee for service Medicare covers like before. Good Luck,
I was put on ALIANCE COMPLETE CARE about a year ago, after I had trouble FINDING A DOCTOR that would accept my FEE-FOR-SERVICE coverage…(I’m a 48 year old disabled woman w/medi-medi)I used my “COMPLETE CARE” coverage TWICE in the years time. WHY? Because there were NO PROVIDERS in my area that I could UNDERSTAND and NO SPECIALISTS to address WHAT is wrong with me! I became disabled in 2004. TEN YEARS LATER, I am in the SAME BOAT!? It looks to me like NEITHER of the “options” available to medi-medis in California are even worth signing up for! I’ll be better off with NO INSURANCE! All I needed was to find a musculoskeletal specialist (if there even IS such) and who knows? I could be ‘fixed’, back working and OFF SS disability! SO, really, WHAT IS THE POINT?