 As California continues the move toward a more coordinated health care system, The SCAN Foundation together with The Department of Health Care Services (DHCS) has released a new report that uses extensive 2008 data to provide insight into the characteristics, needs, service use and costs for Medi-Cal Long-Term Services and Supports (LTSS) recipients in California.
As California continues the move toward a more coordinated health care system, The SCAN Foundation together with The Department of Health Care Services (DHCS) has released a new report that uses extensive 2008 data to provide insight into the characteristics, needs, service use and costs for Medi-Cal Long-Term Services and Supports (LTSS) recipients in California.
View and download the report here.
Prepared by the California Medicaid Research Institute (CAMRI), the analyses in the report allow for a broad, county-by-county look at Medi-Cal program use and spending across the entire continuum of care for people with LTSS needs. This includes LTSS recipients that are dually eligible for both Medicare and Medi-Cal.
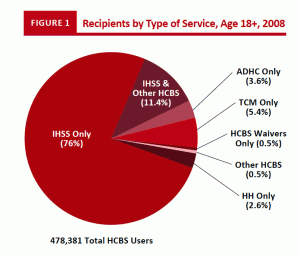
Here are some highlights from the report about the population likely to be affected by the Coordinated Care Initiative in the eight participating counties:
- Minority populations make up the majority of LTSS users across all counties. Women and racial minority groups combine to be a significant portion of recipients of HCBS. Across counties, women accounted for at least 65 percent of HCBS users and racial minorities comprised at least 63 percent of HCBS users. These facts illustrate the necessity of the CCI’s outreach efforts to these populations.
- Most LTSS users are age 65 and older. Across all counties, HCBS users over the age of 65 were at least 51 percent of the consumer population, with percentages of 65 and older recipients reaching as high 67 and 79 percent of HCBS users in Los Angeles and Santa Clara counties respectively.
- LTSS recipients often have high levels of need. More than 90 percent of Medi-Cal LTSS consumers are eligible for services due to receiving public assistance for being aged, disabled, or medically needy. Additionally, at least one quarter of HCBS users across all eight counties have cognitive limitations, with a high of 52 percent in San Mateo County.
- Total public spending was higher for dual eligible LTSS recipients than for Medi-Cal only LTSS recipients. Total spending per recipient for dual eligible recipients across all counties was nearly twice that of the spending for Medi-Cal only recipients. In some counties average spending per dual eligible was as much as eight and ten times higher. Post-acute care was a category of particular disparity in costs between dual eligible and Medi-Cal only consumers.
The report excludes Medi-Cal LTSS users in the Program for All-Inclusive Care for the Elderly (PACE) and those who qualify for services based on a diagnosis of a developmental disability are excluded from the report. Also, in Orange and San Mateo counties, the fee-for-service beneficiaries were a relatively small population due to the existing models of managed care in these counties and the cost data is less representative of the Medi-Cal LTSS population as a whole.
