Dave once was a whiz at chess and had dreams of owning a ranch in the Argentine pampas. Now, he can’t recall his own address and phone number or tell you the day of the week.
Dave, 34, has schizophrenia/schizoaffective disorder. He has been hospitalized several times following manic episodes, but with consistent care, he has remained stable at home in Palm Springs for nearly three years.
Getting the services he needs when he needs them, however, has often been a struggle.
A couple of years ago, when Dave and his life companion, Doug, lived elsewhere in California, Dave had to go to the emergency department just to get a prescription refill of the antipsychotic medications needed to control his hallucinations. He couldn’t get an appointment with a local psychiatrist, even though he has coverage through two public insurance programs – Medicare and Medi-Cal.
The county mental health department said they saw only indigent patients and gave him a list of doctors in private practice. None of those private doctors would see “dual eligible” patients like Dave because getting reimbursed by the two programs can be difficult.
“The way things are set up now,” says Doug, “it feels almost as though it’s about creating loopholes.”
Doug works full-time at home as an online travel coordinator. His other full-time job is taking care of Dave. “He can’t even go to the doctor without me,” Doug says. “He would just be completely lost.”
Dave is one of California’s 1.1 million dual eligibles – people receiving both Medicare and Medi-Cal benefits. Like 30 percent of California’s dual eligibles, Dave qualifies for the public health insurance programs due to his disabling medical condition.
Dave’s services and benefits come through at least four different systems – none of which are coordinated. He now goes to the local county mental health service, which bills Medicare and Medi-Cal to cover his care. His primary care doctor is at a different clinic, and mostly Medicare covers those services. His prescriptions come through a company offering the Medicare Part D drug benefit. Dave also qualifies for the In-Home Supportive Services (IHSS) program that allows Doug to be paid for 40 hours of caring for Dave each month. The County runs the IHSS program, which Doug said is crucial to ensuring that Dave can remain living at home.
The current situation is “very stressful to me,” Doug says. “I have to hold down this job, but he needs me full time. Getting all the bureaucratic entities on the same page would be great.”
When Doug started the process to try and increase Dave’s allotted IHSS attendant hours, for example, he realized Dave’s psychiatrist had never heard of the program. The IHSS and mental health programs didn’t work closely together, and Doug had no one to help him coordinate between the systems. Filling out the paperwork turned into a nightmare that has dragged on unresolved for more than a year.
“The problem is that these different entities don’t converse with each other,” Doug says. “It would be wonderful if the county mental health would be on the same page as IHSS and if the psychiatrist would have (known about IHSS) and taken the time to fill out the form. We’re stuck in the system, and the system seems a little adversarial.”
Doug looks forward to changes that would simplify the system. “It couldn’t be more limited than what we have now.”
Learn More:
Disability Rights California: IHSS Nuts & Bolts

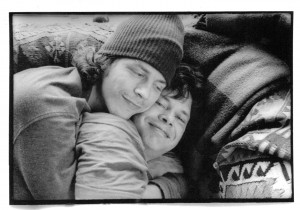
I know Doug & Dave, they’re lovely people. They have good hearts. I’ve spent time with them together and I’ve seen how much they care for each other, and how Doug looks out for Dave.
It’s an inspiring thing to see–without Doug, Dave would be lost, and possibly in an institution.
Doug and Dave deserve the increased benefits. it’s not right that they should have to fight this hard to get them.