Today, the Department of Health Care Services (DHCS) formally announced the California Advancing and Innovating Medi-Cal (CalAIM) proposal at the DHCS Stakeholder Advisory Committee meetings. CalAIM proposes several statewide changes including, but not limited to:
- Requiring Medi-Cal managed care plans to submit Population Health Management strategies and moving to annual Medi-Cal managed care plan open enrollment
- Adding a new Enhanced Care Management benefit and a set of In Lieu of Services
- Behavioral Health payment reform and delivery system transformation
- Requiring National Committee on Quality Assurance (NCQA) accreditation for Medi-Cal managed care plans
- Considerations for creation of Full Integration Plans where one entity would be responsible for the physical, behavioral and oral health needs of their members
Future of Care Integration for Duals
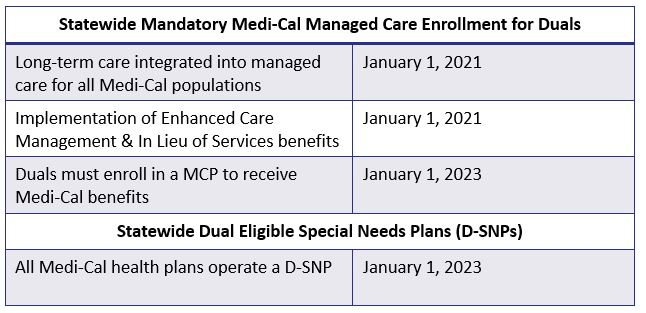
In order to achieve a more standardized approach to comprehensive care coordination for all populations, DHCS is proposing to discontinue the Cal MediConnect pilot program at the end of calendar year 2022. DHCS proposes to transition from the pilot approach of the Coordinated Care Initiative to standardized mandatory enrollment of dual eligibles into a Medi-Cal managed care plan for Medi-Cal benefits and integration of long-term care into managed care for all Medi-Cal populations statewide. This will be done in two phases:
January 2021: The Coordinated Care Initiative proceeds as today, however Multipurpose Senior Services Programs will be carved out and all institutional long-term care services will be carved into managed care for all populations enrolled in plans around the state. DHCS will also implement the voluntary in lieu of services benefit at this time.
January 2023: Full transition of the Coordinated Care Initiative to mandatory managed care enrollment of dual eligibles into managed care in all counties/plan models. In addition, require Medi-Cal managed care plans to operate Medicare Dual-Special Needs Plans, in order to offer dual eligible members the ability to have coordinated managed care plans for both their Medi-Cal and Medicare benefits.
The purpose of these transitions and phases is to target a long-term goal of implementing managed long term services and supports (MLTSS) statewide in Medi-Cal managed care beginning in 2026 by providing enough time and incentive to develop the needed infrastructure. This will allow beneficiaries to receive needed MLTSS and home and community based services statewide through their managed care plan, instead of a variety of 1915(c) waivers that currently have capped enrollment and are not statewide.
The table below shows a timeline of upcoming changes that will impact dual eligibles in California.
For more information on this proposal, visit the DHCS CalAIM website. For any other comments, questions, or concerns, please contact CalAIM@dhcs.ca.gov.

For Developmentally Disabled clients that were not mandated to enroll in Cal Mediconnect, how does this change impact long term care supports for Regional center clients to include Intermediate Care Facilities- DD-H and DD-N? Also, when emergency placements are required for such individuals based on circumstances related to Title 17 compliance issues, what will be the role of MCP’s as well as, that of the Regional Center’s that are mandated by DDS?