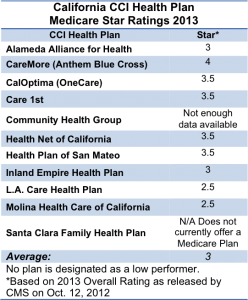
 The Centers for Medicare & Medicaid Services (CMS) announced on October 12 the 2013 quality star ratings for Medicare health and drug plans. The rated plans selected to participate in California’s Coordinated Care Initiative (CCI) received an average rating of 3 out of 5 stars.
The Centers for Medicare & Medicaid Services (CMS) announced on October 12 the 2013 quality star ratings for Medicare health and drug plans. The rated plans selected to participate in California’s Coordinated Care Initiative (CCI) received an average rating of 3 out of 5 stars.
All ratings can be found on Medicare’s Plan Finder at www.Medicare.gov.
Health plan quality in the CCI and across Medi-Cal is a significant focus for the Department of Health Care Services (DHCS). While the star ratings released Friday are a positive data point, they and other quality measures show that there is opportunity for quality improvement. DHCS is committed to its ongoing work with health plans to improve care quality.
To ensure beneficiaries receive high quality care under the CCI, a rigorous quality improvement and quality-monitoring program will be implemented. An external evaluation team will measure, monitor, and evaluate the impact of the State’s demonstration on the cost, quality, and utilization of care received by dual eligible beneficiaries. In addition, DHCS will require that health plans take steps to coordinate care, in accordance with standards developed by the National Quality Forum.
These efforts are summarized in two new fact sheets on the duals demonstration evaluation and CCI quality monitoring process.
Medicare Star Rating Background
The 5-star rating system is used by CMS to monitor plans to ensure that they meet Medicare’s quality standards. The ratings provide Medicare beneficiaries with a tool to compare the quality of care and customer service that Medicare health and drug plans offer. CMS’ star rating system considers 53 quality measures, such as success in providing preventive services, managing chronic illness, and keeping consumer complaints to a minimum. A “low performer” icon is to be placed next to the names of plans that have received less than three stars for the past three years.

Amazing how improved the health plans have suddenly improved! Maggie