To provide a greater understanding of the Medicare-Medicaid enrollee or “dual eligible” population, CMS developed profiles that examine this population’s demographic characteristics, utilization, and spending patterns on a state-by-state basis. All 50 state profiles can be found here.
You can download California’s profile, but here is a closer look at the data compiled about the state’s dual eligible beneficiaries. The primary data source for the tables below is linked Medicare and Medicaid administrative and claims data for persons age 18 and older from calendar year 2007.
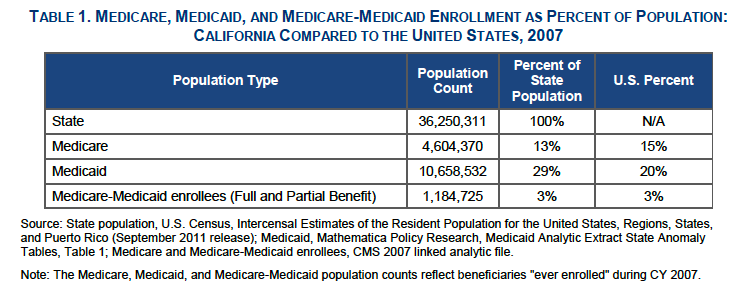
Total Population
Eligibility
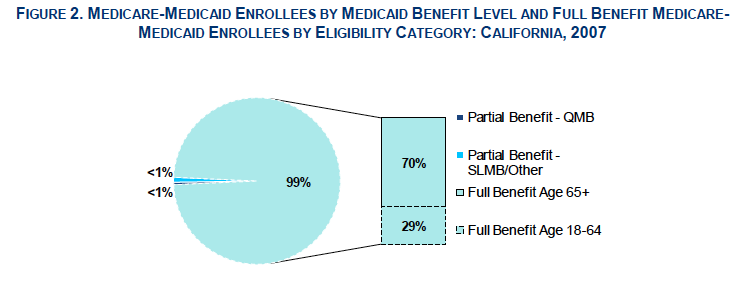
In California, 99% of dual eligible beneficiaries had full Medi-Cal benefits: 70% were ages 65 and older and 29% were ages 18 to 64. The remaining “partial benefit” enrollees received Medi-Cal help with Medicare premium payments and/or Medicare cost-sharing.
Demographics
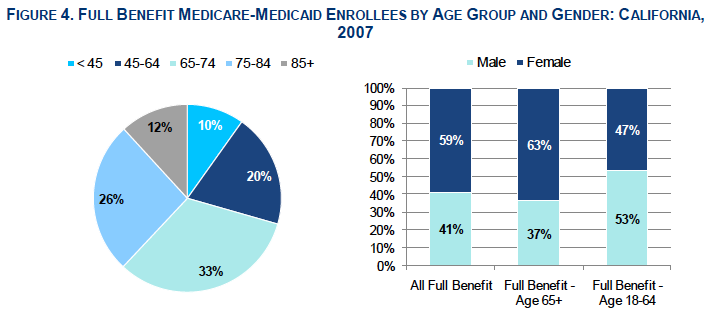
A total of 71% of full benefit enrollees in California were age 65 and older; people age 85 and older comprised 17% of this group. The majority of full benefit enrollees in California were women, particularly among the 65 and older group.
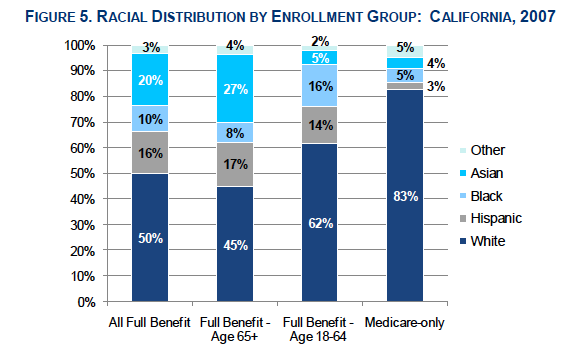
The dual eligible population is racially diverse. More full benefit dual eligible enrollees were non-white compared to the Medicare-only population.
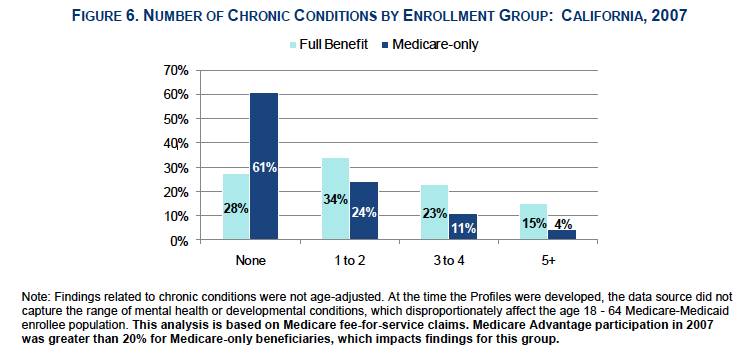
Chronic Conditions
Dual eligible beneficiaries have numerous chronic health conditions and tend to be sicker than the the Medicare-only population. Dual eligible enrolless were 3.5 times more likely than Medicare-only beneficiaries to have had 5 or more chronic conditions.
Utilization
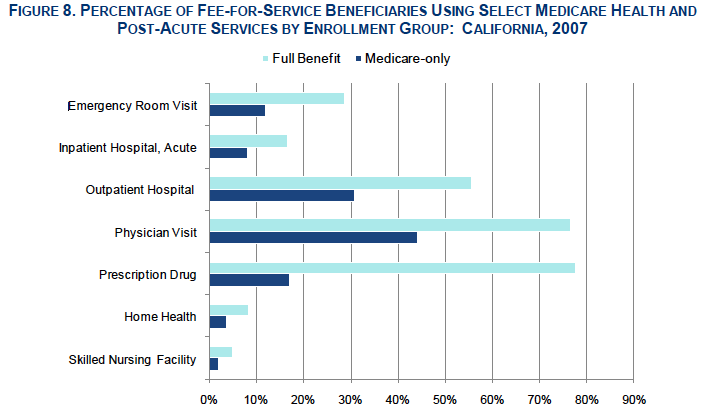
Dual eligible beneficiaries have, on average, greater health and long-term services and supports (LTSS) needs than beneficiaries who have only Medicare or only Medicaid coverage. Dual eligible beneficiaries accounted for a disproportionate share of total utilization and spending in both programs.
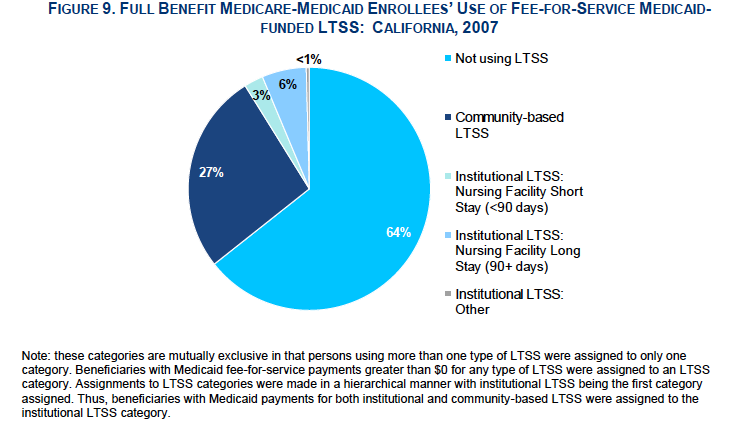
The majority of dual eligible in California did not use Medi-Cal-funded long-term services and supports. Of those who did, 75 percent used community-based LTSS and the remainder used institutional long-term care.
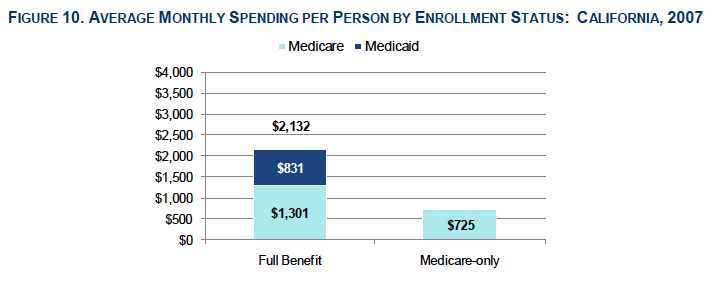
Spending
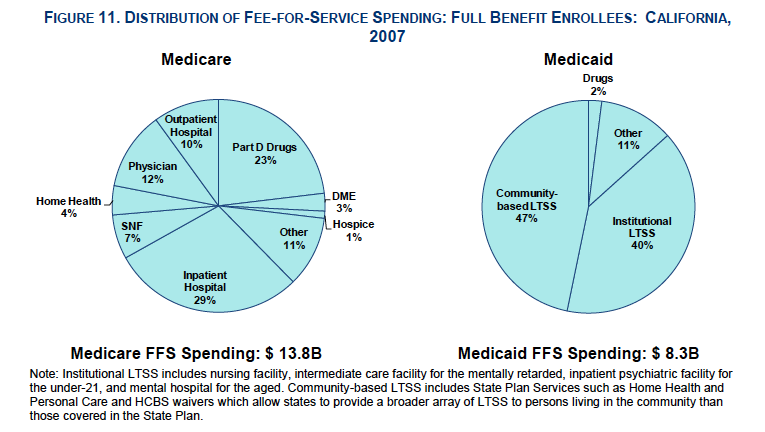
Dual eligible beneficiaries had significantly higher average monthly spending per person compared to Medicare-only beneficiaries, including higher average Medicare costs. Total costs included managed care and fee-for-service payments. The largest share of dual eligible beneficiaries fee-for-service Medicare spending went toward inpatient hospital care, whereas the largest share of fee-for-service Medi-Cal spending went toward long-term care services.